
A solution to reduce your claims rejection
Group of trained RCM professionals (internal or outsourced) who are involved with the patient from the start of their care to the very end when payment is made. They assign appropriate codes based on a patient's record and bill. These codes are made into Pre-approval & claims that are sent to the patient’s insurance company/TPA. Though RCM unit use professional team, still claim rejection persist, and it is mainly due to gap between patient EMR and RCM process and leads to following rejections:
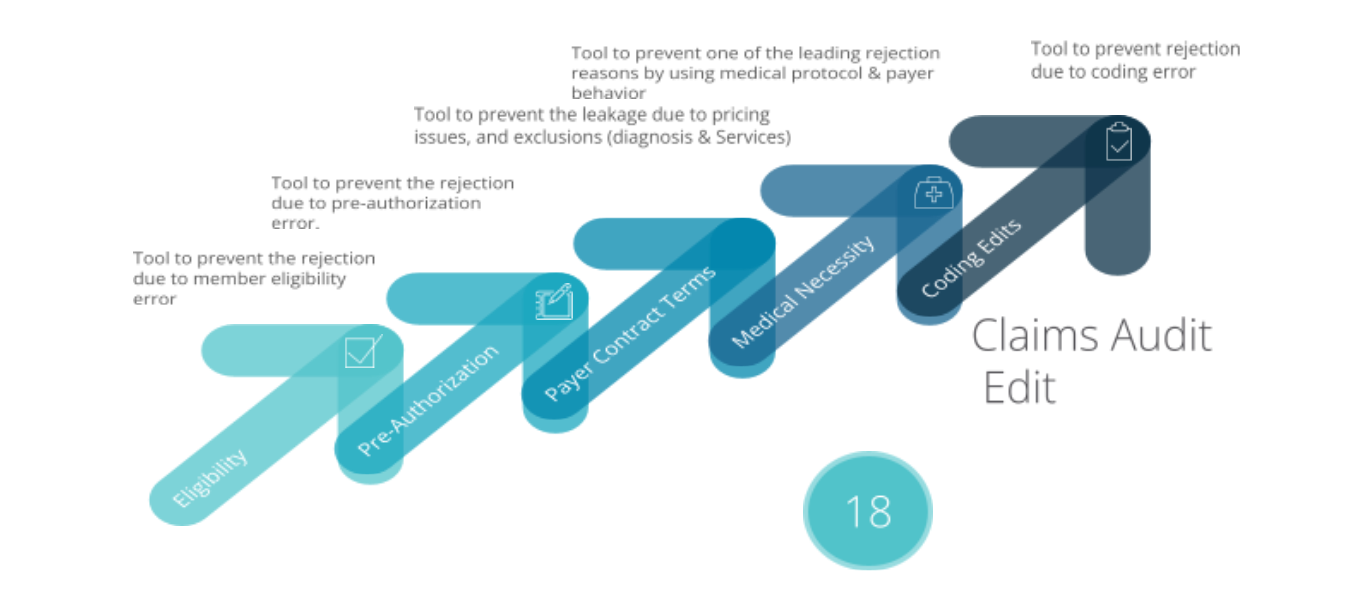
Cephal offers a Claims Pre-submission Tool is to identify potential reject-able claims and guide healthcare providers to rectify the gap prior to claim submission. Tool address the following errors and flag them for correction.
Other
Services
Our Services
Data Clearing House
Cephal Healthcare Data Clearinghouse provide the ability to take in non-standard data and process it into standard data formats that can be ingested into any pertained regulatory bodies, insurance payers, healthcare Analytical tools…etc.
Data Cleansing
Cephal Data cleansing or data cleaning is to detect and correct corrupted or inaccurate records from patient record set, table, or database and refers to identifying incomplete, incorrect, inaccurate or irrelevant parts of the data and then replacing, modifying, or deleting the dirty or coarse data.
Revenue Cycle Management System
Revenue Cycle management (RCM) is the financial process between healthcare providers and insurance payers, where utilizing the right RCM technical tool and process that facilitates to process the claims activities more efficiently and effectively.
Revenue Cycle Management - Operation
Along with RCM system, equally important to have an experienced medical coders and other supporting RCM operational resources for effective RCM outcome.
Pharmacy Benefit Management
Cephal Pharmacy Benefit Management is an automated Clinical Screening Solution, using technology to support clinicians with making better informed medication-related decisions. It is designed to alert clinicians and pharmacists making prescribing decisions to information about avoidable medication errors, inappropriate dosing and adverse events.
Claims Analytics - Medical Data Analytics
For Healthcare providers, revenue cycle management is an integral - but complicated component of ensuring an organization runs efficiently and effectively.
Medical coding and Audit Tool
Medical coding can be incredibly laborious to assign medical codes. The complexity of the medical coding process has increased due to the latest healthcare reforms. There is demand for perfect documentation and its coding. Anything less than perfect, means, rejected claims, or, worse still, fines for miscoding.







